We live in a world of consumerism and companies are ever-increasingly focused on doing more to satisfy their customers. However, healthcare is different as a customer is not a typical value or experience seeker, but a patient in need of care. Healthcare in most countries is a fundamental right of an individual, and one of the core tenets of evolution and progress. And hence, every year all the stakeholders including the government, academic and research institutes, pharma and medical device companies, hospitals and the public pour crores into research and identification of solutions for better care.
As all these stakeholders focus on innovation and the next-best thing in healthcare, one must ask if the problem of improving patient care and health outcomes is truly being solved. Every year India sees innovative solutions either driven indigenously or imported from other countries and contextualized for the local healthcare system. However, most of these solutions providers given the siloed nature of the industry take a very microscopic view of the disease, trying to solve for one pain point through their product or service. We have identified a couple of simple yet commonly observed case-studies to highlight the problem and share a patient-perspective as they interact with these innovative solutions, developed to help improve their condition and quality of life.
Case-study I: An elderly patient on regular dialysis
Let’s take a case of an elderly patient having diabetes and related kidney failure and requiring dialysis on a regular basis. The doctor will do everything he or she can by prescribing the right care, regular procedures and follow-ups. However, there are other facets to the disease management and things that a patient can do himself or herself as well such learning more about the disease, precautions, side-effects, adhering to a regular medicine schedule, regularly measure hemoglobin levels as they tend to deteriorate over time, work with a dietitian on an adequate meal plan and so on.
As we look at these challenges, there are multiple solutions that are presented to the patient including reminder apps for improving compliance, lifestyle management application for diabetes management, diary to maintain a regular log of hemoglobin control, or a home-based hemoglobin measurement device (like the home-based glucometer). As we look at these many great solutions from a patient perspective, a few natural questions that emerge are: (a) how many applications and devices can a single patient manage? (b) how does all the data come together from these multiple solutions, and (c) what if the patient has other disease which hasn’t been covered as part of these disease management solutions?
Case-study II: A child suffering from Juvenile Idiopathic Arthritis
Juvenile or childhood arthritis is a condition where a child undergoes bouts of painful swelling inflammation of joints. While the course of treatment is relatively well-established including physical therapy, pain-killers, corticosteroids, DMARD’s and surgery in some rare cases, given the young age of the patient there are multiple open questions that remain to be answered: (a) how do you motivate the child to get regular physical therapy, (b) how do you alleviate the pain during treatment and, (c) also how do you support the education of the patient during this journey?
With today’s technology evolution such as introduction of gamification in healthcare, digital patient education platforms, and virtual reality to help combat pain, the future of this treatment looks promising. Stakeholders will have to however work on building a holistic ecosystem and not siloed solutions using the foresaid technologies, ensure that the experience for the child remains personalized and more importantly humanized, and continuously ensure that all this eventually leads to improvement of clinical outcomes.
During past few years of my experience in studying the patient journey for various diseases, evolution and deployment of various innovative solutions and the unmet needs, I have realized that there are four key elements that define any patient-centric solution:
- Information / Engagement: Quality of information shared, and the degree of engagement achieved with the patient
- Channels: Select the most appropriate and effective channel for each activity
- Patient Journey: Ability to engage at each stage of patient journey and bring the right value proposition
- Personalization: Personalization or customization of the services to the extent possible and in the right context
Below map indicates a reference framework for identifying different pain-points and areas of considerations as we design a solution for any disease area.
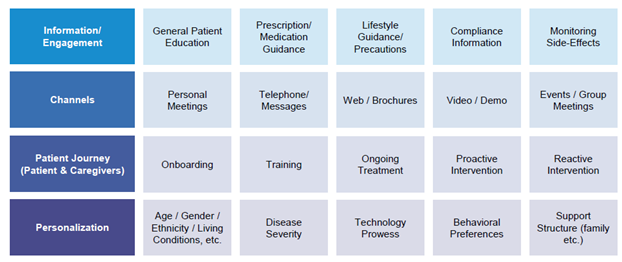
Stakeholders need to consider the following factors and answer related questions such as:
- Information / Engagement: Are we enabling the patient with all the information and engagement aspects across the spectrum? A pharma company might be more inclined to share prescription guidance and a dietitian might be more inclined to share only a meal plan, but then such an approach would mean that the patient must shop around the ecosystem to for information
- Channels: What are the right channels for disseminating the information amongst the available options? Each provider might not have all the channels, but there are ample opportunities to collaborate and ensure the right channel partner is involved
- Patient Journey: What stage of the disease journey is the patient going through, and based on that are we addressing the right needs of the patient and the care-giver?
- Personalization: Does the solution require personalization, humanization and contextualization based on the various outlined parameters?
During introduction of the recent healthcare reforms in US, one of the most emphasized roles was that of a ‘care coordinator’, someone who can stitch a holistic experience for the patient. We seeing some interesting solutions being introduced in India as well for 360-degree management of diabetes and a few other chronic diseases, which include delivering the medication to the patient on time, timely reminders, education on using the insulin pen correctly, diet advice, answering any other queries the patient has, lifestyle guidance and counseling. While most stakeholders do not have all the capabilities internally, the most encouraging sign is that they are collaborating with each-other with one common goal of helping the patient. Are you working towards the same?





